Just Care for Dementia in Prison
A research team from The Penn State University Ross and Carol Nese College of Nursing and Klein Buendel made two presentations related to formative research on the development of Just Care for Dementia at the 36th Annual Scientific Sessions of the Eastern Nursing Research Society April 4-5, 2024 in Boston, MA.
Presentation 1
Title: Dementia Care Training Needs for Corrections Staff and Peer Caregivers

Presenter: Dr. Susan Loeb
The number of people living in prison with Alzheimer’s Disease and Related Dementias (ADRD) is growing. Care inequities for ADRD between prisons and community settings exist and warrant addressing. A standardized, evidence-based, feasible, and acceptable ADRD e-training program is needed to prepare corrections staff and peer caregivers for better managing and caring for people with ADRD in prisons.
The purposes of this study were to (1) identify three priority learning needs of corrections staff and peer caregivers who manage and/or care for people living with ADRD in prisons; (2) identify a logo for the Just Care for Dementia training that was desirable to end-users; and (3) translate best practices from community-based ADRD care into evidence-based, accessible, and relevant ADRD content for prison settings. The end goal was to program prototypes for three highly interactive e-learning modules that fit within the restrictive context of corrections.
Focus group methodology guided potential future users in providing insights to ensure the content, design, and technology plans match the needs and constraints of prisons. Human subjects approvals were secured and participants’ signed informed consent was obtained. Settings were one men’s and one women’s state prison in the northeastern United States. Twelve corrections staff and 11 peer caregivers participated. Focus groups were audio recorded, transcribed, and deidentified.
Thematic analysis was completed independently by two researchers. The three priority content areas identified were fostering a safe and calm environment, addressing behavioral and psychological symptoms of dementia, and enhancing awareness of need. Participants identified two logo preferences. Advisory board consultation informed logo selection. Module content was developed via an iterative process to ensure contextual relevance of training, accessibility within the constraints of prisons, and the e-training matched identified training needs.
In summary, participants confirmed the need for ADRD training and indicated e-learning is a viable approach for addressing a pressing care need in prisons.
This research was funded by an STTR grant to Klein Buendel from the National Institute on Aging (AG057239; Dr. Susan Loeb from Penn State and Dr. Barbara Walkosz from Klein Buendel, Multiple Principal Investigators). Collaborators included Dr. Erin Kitt-Lewis and Sherif Olanrewaju from Penn State University; and Amanda Brice and Steve Fullmer from Klein Buendel.
Presentation 2
Title: Small-Scale Usability Testing: E-learning modules for Peer Caregivers
Presenter: Dr. Susan Loeb
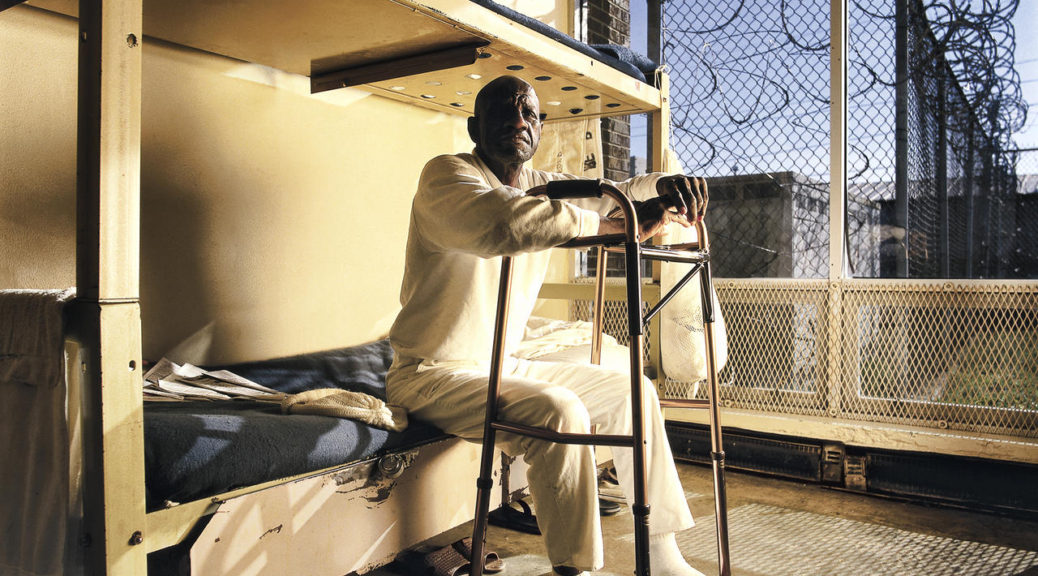
Growing numbers of people will grow old and die while incarcerated. Research evidence supports using peer caregivers to assist staff with geriatric and end-of-life care. Peer caregivers training varies widely in content and duration. Evidenced-based, accessible, and contextually relevant materials are needed to effectively prepare peer caregivers.
The purpose of this study was to conduct research and development for Just Care, a six-module e-learning program for peer caregivers and a single module to guide corrections staff in launching the program. Deputy Wardens identified people meeting our inclusion criteria. Nineteen people living in prison and 11 staff participated. Throughout usability testing, participants shared their thoughts aloud, while field notes were taken. Participants completed six open-ended questions, a demographic survey, and the System Usability Scale (SUS).
All users easily navigated through the program with minimal guidance. Many noted Just Care’s utility for future peer caregivers. Some users who were incarcerated had difficulty navigating the post-test assessments. A few staff users noted liking the additional resources available via links to PDFs. One staff user voiced concern about the safety of having incarcerated people help with care. Just Care received Round 1 SUS scores of 87.5 by users living in prison and 74.5 by staff. Following rapid refinement, Just Care received Round 2 mean SUS scores of 85.28 by users living in prison and 83.75 by staff. A SUS score of 68 is an above average score.
Overall, participants found Just Care innovative, useful, engaging, interactive, and relevant to providing geriatric and end-of-life care in prisons. Staff noted that Just Care raised awareness about the growing need for programming on geriatric care in prisons and that a peer caregiver program is a viable solution that is implementable by prison staff.
This research was funded by an STTR grant to Klein Buendel from the National Institute on Aging (AG057239; Dr. Susan Loeb from Penn State and Dr. Barbara Walkosz from Klein Buendel, Multiple Principal Investigators). Collaborators included Dr. Erin Kitt-Lewis and Sherif Olanrewaju from Penn State University; and Brandon Herbeck, Peter Fu, and Steve Fullmer from Klein Buendel.