#4Corners4Health: Protocol for a Randomized Stepped-Wedge Trial
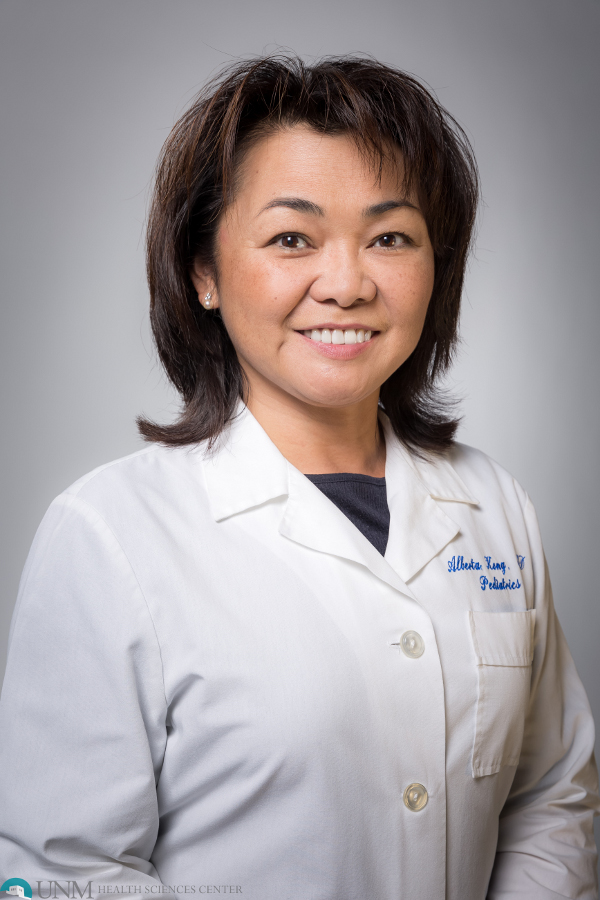
Dr. David Buller from Klein Buendel and Dr. Andrew Sussman from the University of New Mexico are leading a large multiple state research team on the design, implementation, and evaluation of #4Corners4Health. The research study aims to decrease cancer risk factors among emerging adults (ages 18-26) living in rural counties in the Four Corners states of Arizona, Colorado, New Mexico, and Utah using a targeted social media campaign. The team has published a full description of their study procedures in JMIR Research Protocols.
Many emerging adults are prone to making unhealthy choices, which increase their risk of premature cancer morbidity and mortality. In the era of social media, rigorous research on interventions to promote health behaviors for cancer risk reduction among emerging adults delivered over social media is limited. Cancer prevention information and recommendations may reach emerging adults more effectively over social media than in settings such as health care, schools, and workplaces, particularly for emerging adults residing in rural areas.
Specifically, the research team will recruit a sample of 1000 emerging adults aged 18 to 26 years residing in rural counties in the Four Corners states from the Qualtrics’ research panel and enroll them in a randomized stepped-wedge, quasi-experimental design. The inclusion criteria include English proficiency and regular social media engagement. A social media intervention will promote guideline-related goals for increased physical activity, healthy eating, and HPV vaccination and reduced nicotine product use, alcohol intake, and solar UV radiation exposure. Posts will cover digital and media literacy skills, responses to misinformation, communication with family and friends, and referral to community resources. The intervention will be delivered over 12 months in Facebook private groups and will be guided by advisory groups of community stakeholders and emerging adults and focus groups with emerging adults. The emerging adults will complete assessments at baseline and five additional data after randomization. Assessments will measure six cancer risk behaviors, theoretical mediators, and participants’ engagement with the social media campaign.
The trial is being led by a steering committee. Team members are working in three subcommittees to optimize community engagement, the social media intervention, and the measures to be used. The Stakeholder Organization Advisory Board and Emerging Adult Advisory Board were formed and provided initial input on the priority of cancer risk factors to target, social media use by emerging adults, and community resources available. A framework for the social media intervention with topics, format, and theoretical mediators has been created, along with protocols for social media management.
In summary, the researchers believe that social media can be used as a platform to counter misinformation and improve reliable health information to promote health behaviors that reduce cancer risks among emerging adults. Because of the popularity of web-based information sources among emerging adults, an innovative, multiple risk factor intervention using a social media campaign has the potential to reduce their cancer risk behaviors.
This research is supported by a 5-year R01 grant from the National Cancer Institute (CA268037) to Klein Buendel. Dr. David Buller from Klein Buendel and Dr. Andrew Sussman from the University of New Mexico are the project’s Multiple Principal Investigators. The JMIR publication has 24 collaborating authors from multiple institutions.