Immersive STAC Luminary Presentation
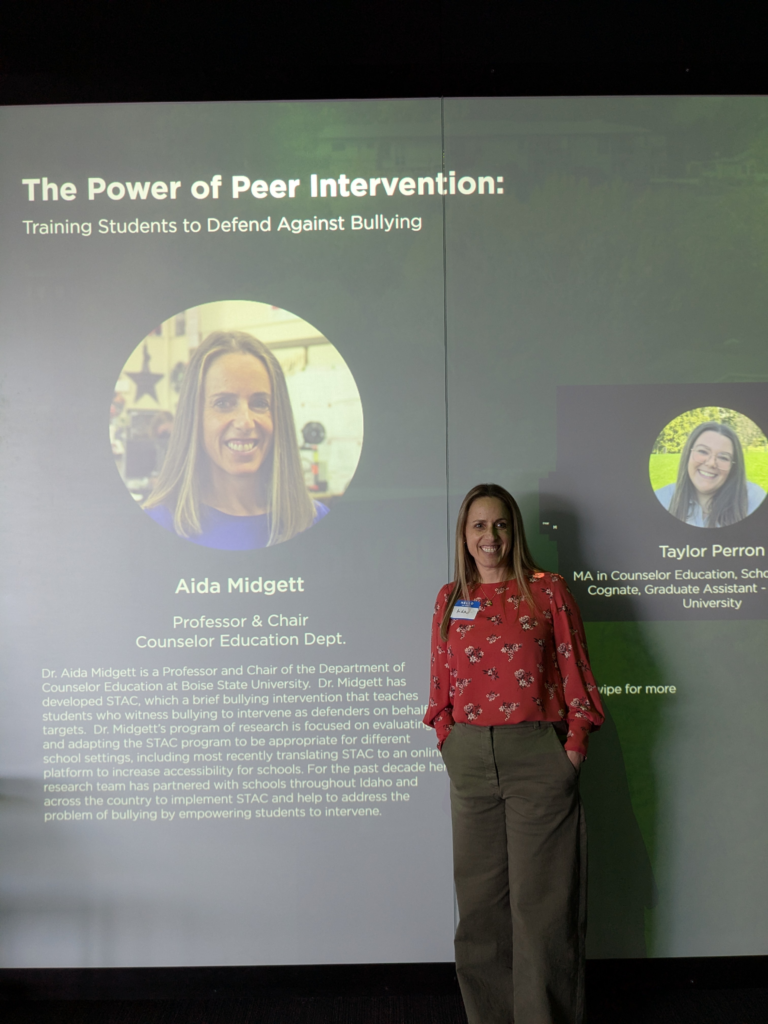
The imaginative illustrations and digital production work of the Klein Buendel Creative Team were featured in a life-size immersive luminary display in the Keith and Catherine Stein Luminary at Boise State University in April.
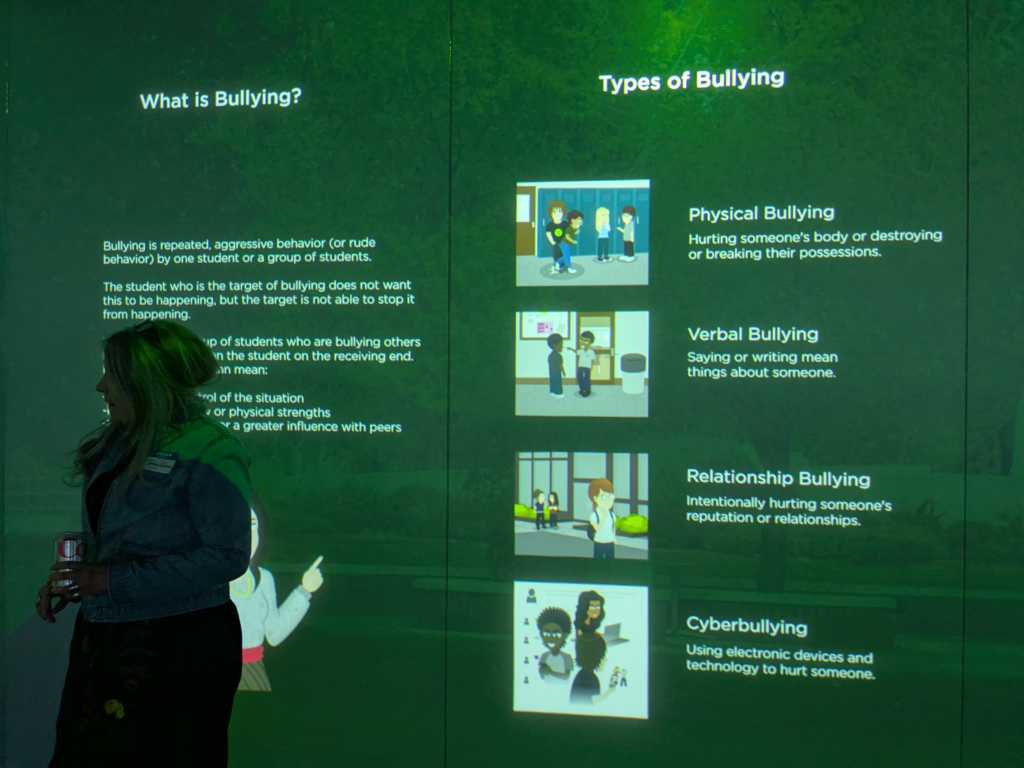
The STAC intervention, developed by Dr. Aida Midgett from Boise State University, was the subject matter on full display. STAC provides middle school students who witness bullying with strategies to act as “defenders” to help reduce both active bullying and the negative associated outcomes for both targets and bystanders. The content is delivered in person or via web-based lessons and activities which includes avatar-based scenarios, practices, and quizzes.

STAC Bullying Bystander Strategies
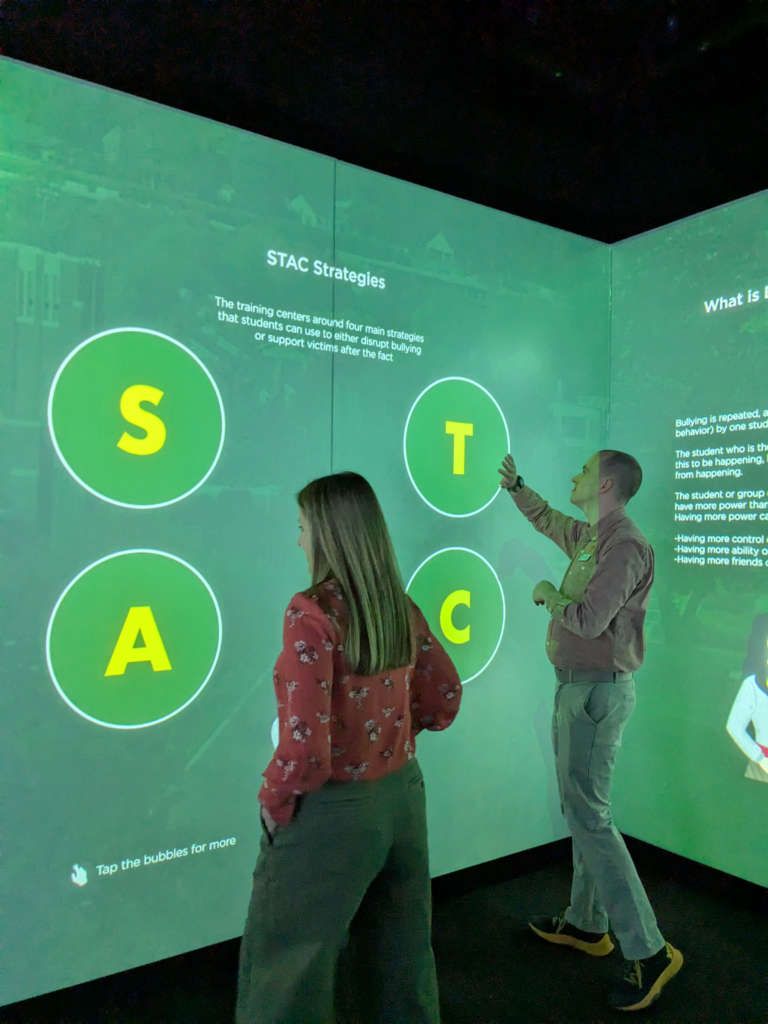
(1) “Stealing the Show” – using humor or distraction to interrupt a bullying situation and remove the attention away from the target;
(2) “Turning it Over” – identifying a trusted adult at school, reporting, and asking for help during a bullying incident;
(3) “Accompanying Others” – befriending and/or providing support to a peer who was a target of bullying; and
(4) “Coaching Compassion” – gently confronting the perpetrator and increasing empathy for the target.
The research to design and evaluate the interactive web-based version of STAC is funded by an STTR Phase II grant to Klein Buendel from the National Institute on Minority Health and Health Disparities at the National Institutes of Health (MD014943; Dr. Aida Midgett, Principal Investigator, Boise State University). Co-investigators include Dr. Diana Doumas from Boise State University and Mary Buller from Klein Buendel. The web-based STAC modules were designed and programmed by Klein Buendel’s Creative Team: Steve Fullmer, Creative Director; Peter Fu, Illustrator and Developer; Charlie Barger, Developer; and Brandon Herbeck, Project Coordinator.
The Stein Luminary is an all-digital museum space at Boise State University that produces a variety of immersive, interactive, and sensory experiences. Touch-activated screens and immersive projection deliver cutting-edge visual content for the Boise State University community. According to their website, “The Stein Luminary invites the Boise State community to explore creative arts, cultural sites, and scientific phenomena from around the globe. We foster interdisciplinary collaboration and research-based innovation by featuring exhibitions, performances, and installations of emerging media. Our participatory content generates vital and meaningful conversations about arts, humanities, technology, and science.”
As illustrated in the luminary, the STAC program has been implemented in middle schools across the United States and multiple other countries worldwide.