2024 Research Highlights
Klein Buendel scientists and staff continued to pursue rigorous behavioral science research with multiple national and international collaborators to positively impact the health and safety of people’s lives. Our creative team designed and engineered engaging web-based programs for many of the projects.
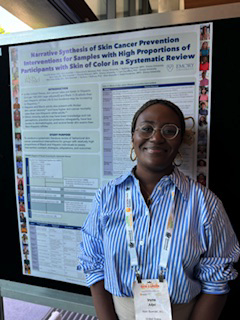
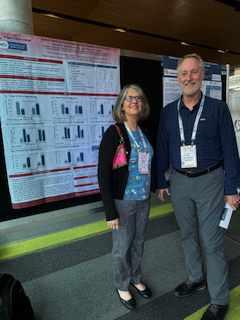
In 2024, we started two new large research projects with current collaborators. We co-authored 11 papers published in peer-reviewed journals or published online ahead of print, including one in the American Journal of Public Health. We presented study results at five national or international conferences, including the 6th International Conference on UV and Skin Cancer Prevention in Brisbane, Australia, where we were awarded the Best Poster prize along with our research collaborator, Emory University.
In February, Dr. Gill Woodall gave a presentation at the University of New Mexico Comprehensive Cancer Center entitled, “Randomized Trials of HPV Vaccine Uptake Improvement in New Mexico: Web Apps for Parents and Young Adolescent Girls and Boys.”
In May, Dr. David Buller gave a presentation for the ACCORDS Dissemination and Implementation Science Program at the University of Colorado Anschutz Medical Campus. His presentation was entitled, “Novel Adaptation of an Evidence-based Occupational Sun Safety Program for Today’s Outdoor Worker.”
In October, Dr. David Buller was an invited presenter on a panel discussion on increasing scale-up research in cancer control, sponsored by the National Cancer Institute. His presentation was entitled “Using Technology to Scale-up and Occupational Sun Protection Program.”
Projects Launched in 2024
- “Emotion Regulation Intervention to Prevent Substance Use Among Youth in the Child Welfare System.” An R61 award to Klein Buendel from the National Institute on Drug Abuse (DA059785; Dr. Chris Houck, Principal Investigator, Rhode Island Hospital). The primary Co-Investigator from Klein Buendel is Ms. Julia Berteletti.
- “Hybrid Delivery to Increase Access and Sustainability: Evaluating ezParent Implementation.” A Fast Track STTR grant to Klein Buendel from the National Institute (HD116627; Dr. Susan Breitenstein, Principal Investigator, Ohio State University). The primary Co-Investigator from Klein Buendel is Ms. Julia Berteletti.
2024 Publications*
- Woodall WG, Buller DB, Saltz R, Martinez L. Professional development to improve responsible beverage service training: formative research results and protocol for a randomized controlled trial. JMIR Res Protoc. 2024 Jan 24:13:e49680. doi: 10.2196/49680.
- Breitenstein SM, Berteletti J, Smoske S, Barger C, Tipps K, Helsabeck NP. Administrative dashboard for monitoring use of a web-Based parent training intervention: usability study. JMIR Form Res. 2024 Jan 30:8:e53439. doi: 10.2196/53439.
- Buller DB, Sussman AL, Thomson CA, Kepka D, Taren D, Henry KL, Warner EL, Walkosz BJ, Woodall GW, Nuss K, Blair CK, Guest DD, Borrayo EA, Gordon JS, Hatcher J, Wetter DW, Kinsey A, Jones CF, Yung AK, Christini K, Berteletti J, Torres JA, Perez EYB, Small A. #4Corners4Health social media cancer prevention campaign for emerging adults: protocol for a randomized stepped-wedge trial. JMIR Res Protoc. 2024 Feb 22:13:e50392. doi: 10.2196/50392.
- Wu YP, Stump TK, Hay JL, Buller DB, Jensen JD, Grossman D, Shen J, Haaland BA, Jones J, Tercyak KP. Protocol for a cluster-randomized trial of a school-based skin cancer preventive intervention for adolescents. Contemp Clin Trials. 2024 May:140:107494. doi: 10.1016/ j.cct.2024.107494.
- Hay JL, Wu Y, Schofield E, Kaphingst K, Sussman AL, Guest DD, Hunley K, Li Y, Buller DB, Berwick M. Exploring the role of cancer fatalism and engagement with skin cancer genetic information in diverse primary care patients. Psychooncology. 2024 Apr;33(4):e6331. doi: 10.1002/pon.6331.
- Buller DB, Woodall WG, Saltz R, Martinez L, Small A, Chirico N, Cutter GR. Sales to apparently intoxicated customers in three states with different histories of responsible beverage service training. J Stud Alcohol Drugs. 2024 May;85(3):312-321. doi: 10.15288/jsad.23-00258
- Kitt-Lewis E, Loeb SJ, Walkosz BJ, Olanreqaju SA, Herbeck B, Fullmer S. Just Care: usability testing of e-learning modules for peer caregivers living in prison. J Offender Rehabil. 2024 Jul;63(6):387-400. Doi: 10.1080/10509674.2024.2370289.
- Buller DB, Buller MK, Meenan R, Cutter GR, Berteletti J, Henry KL, Kinsey A, Adjei I, Chirico N. Implementation of an occupational sun safety intervention: comparison of two scalability strategies. J Occup Environ Med. 2024 Oct 10. doi: 10.1097/JOM.0000000000003248. Online ahead of print.
- Wu YP, Brunsgaard EK, Siniscalchi N, Stump T, Smith H, Grossman D, Jensen J, Buller DB, Hay JL, Shen J, Haaland BA, Tercyak KP. Challenges and lessons learned in recruiting participants for school-based disease prevention programs during COVID-19. Contemp Clin Trials Commun. 2024 Nov 24:42:101399. doi: 10.1016/j.conctc.2024.101399. eCollection 2024 Dec.
- McCrady BS, Woodall WG, Berteletti J, Starling R, Martinez L, Westerberg V, Brooks M, Starke T. Developing a smartphone web app to help DWI offenders and their families. J Subst Use Addict Treat. 2025 Jan:168:209565. doi: 10.1016/j.josat.2024.209565. Online ahead of print.
- Buller DB, Berteletti J, Heckman C, Schroth K, Geller AC, Stapleton JL, Adjei I, Mitarotondo A, Guild SR, Gershenwald JE, Dellavalle R, Pagoto S. Bills to Restrict Access to and Harm from Indoor Tanning Facilities in US State Legislatures, 1992–2023. Am J Public Health. Online ahead of print 10.2105/AJPH.2024.307894.
*KB investigators and staff are indicated in bold type
2024 Conference Presentations
Several presentations on research progress, procedures, analyses, and outcomes were given by Klein Buendel scientists, staff, and their collaborators at the following national and international conferences:
- 45th Annual Meeting of the Society of Behavioral Medicine (March)
- 36th Annual Scientific Sessions of the Eastern Nursing Research Society (April)
- 47th Annual Scientific Meeting of the Research Society on Alcohol (June)
- 6th International Conference on UV and Skin Cancer Prevention (September)
- 36th International Papillomavirus Conference (November)
Klein Buendel and Emory University won Best Poster at the UV Conference in Australia for “Narrative Synthesis of Skin Cancer Prevention Interventions for Samples with High Proportions of Participants with Skin of Color in a Systematic Review.” The poster was presented by Ms. Irene Adjei from Klein Buendel.