E-learning modules for peer end-of-life caregivers living in prison
A research team led by Dr. Susan Loeb from Penn State University and Dr. Barbara Walkosz from Klein Buendel, has published results from a recent study in the Journal of Offender Rehabilitation. The paper reports findings from the usability testing of the Just Care electronic learning program for training carefully vetted people living in prison to assist staff with geriatric and end-of-life care.
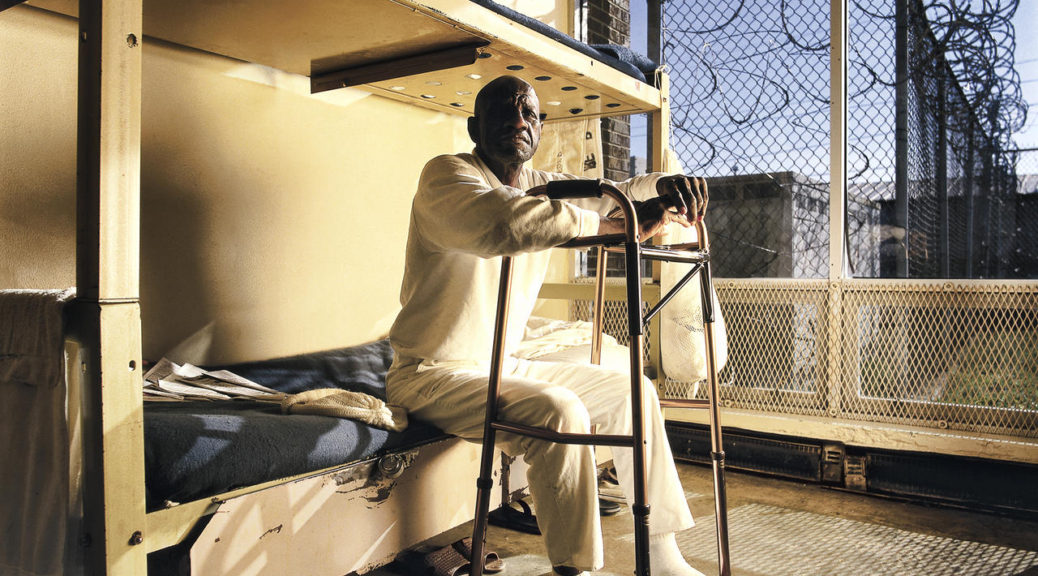
Aging is accompanied by an increased probability of health problems and subsequent need for health care. According to the authors, “The growing number of older adults living in prison, who will likely age and die in prison, calls attention to the challenge of how correctional facilities will care for this population’s health needs, which includes the increasing demand for geriatric and end-of-life care.” Training men and women who live in prison to assist corrections staff with the care of growing numbers of older, sicker, cognitively impaired, and dying people in prison is an innovative and viable option to help meet pressing care demands.
Two rounds of usability testing were conducted via videoconference. Prison personnel (such as corrections specialists, supervisors, nurses, and chaplains) and people living in prison were recruited from one men’s prison and one women’s prison. Fifteen participants completed the testing in each of two rounds. Methods and analyses are described in the paper.
Results include participant demographics, concerns and areas for improvement by severity level of programming, and mean scores for both participant groups on the System Usability Scale. Overall, both the incarcerated and staff participants found the program easy to navigate and the interactive content was useful, engaging, and relevant to caring for incarcerated aging and dying people. The findings helped refine Just Care before additional evaluation was conducted with a larger sample.
This research was funded by an STTR grant to Klein Buendel from the National Institute on Aging (AG057239; Dr. Susan Loeb and Dr. Barbara Walkosz, Multiple Principal Investigators). The lead author on this Journal of Offender Rehabilitation paper is Dr. Erin Kitt-Lewis from Penn State University. Additional authors are Dr. Susan Loeb and Mr. Sherif Olanrewaju from Penn State University; and Dr. Barbara Walkosz, Mr. Brandon Herbeck, and Mr. Steve Fullmer from Klein Buendel.