Dissemination & Implementation Conference
Three occupational sun safety projects were presented by collaborating researchers from Klein Buendel and Emory University at the 16th Annual Conference on the Science of Dissemination and Implementation in Health held December 10-13, 2023, in Washington, DC. Each presentation complemented the conference theme of “Raising Expectations for Dissemination & Implementation Science: Challenges and Opportunities,” by approaching occupational skin cancer prevention in a unique and challenging way.
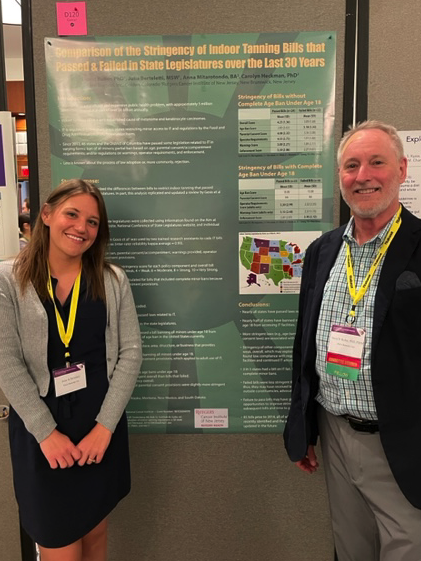
Poster 1
Title: Differences in Program Implementation and Sun Protection of an Occupational Sun Safety Intervention: Comparison of Two Dissemination Strategies
Presenter: Dr. David Buller, Klein Buendel
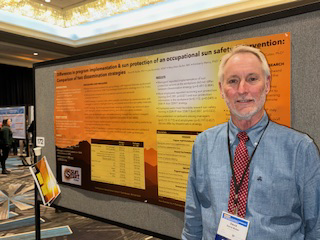
Balancing effectiveness and cost is essential when scaling up evidence-based interventions. In this study, two methods for disseminating an evidence-based occupational sun protection intervention that differed in cost and personal contact were compared. Solar ultraviolet radiation is a carcinogen associated with skin cancer.
Sun Safe Workplaces (SSW), a policy and education intervention, was effective in a randomized trial in Colorado (1,2). Two methods for disseminating SSW were compared in a randomized pretest-posttest two-group trial design. State departments of transportation (DOTs; n=21) participated and the 136 districts within these DOTs were randomly assigned to receive SSW either by an in-person coaching method or a virtual coaching method. In each district, managers were pretested prior to randomization (n=1,484) and posttested (n=289) after 29-40 months (timing and attrition were affected by the COVID pandemic) on implementation of SSW training and communication and personal sun protection practices. Employees (n=1,388) also were posttested on training and communication implementation and personal sun protection practices.
There was no difference in managers’ reported implementation of sun protection actions at the workplace between dissemination methods. But more employees reported receiving sun protection training in in-person (60%) than virtual (46%) dissemination method and being more favorable toward this training (in-person M=3.70, virtual M=3.60.) Managers at workplaces receiving SSW via in-person dissemination experienced fewer sunburns in the past year while working outdoors than with virtual program delivery (M=0.69 v. M=1.58 sunburns; estimate=-0.875, p<0.011), especially at workplaces receiving it before the pandemic compared to later in the pandemic (in-person=0.43, virtual=0.79).
Effectiveness of evidence-based programs when scaled-up may be affected by the method of dissemination. Here, in-person coaching may have increased implementation of SSW training. It also may have aided coaches in convincing managers that there was a need for occupational sun safety and motivated them to avoid sunburn themselves and work to make employees see the value in training. The virtual delivery method may not have affected employees’ personal protection because they had limited contact with the coaches. Pandemic restrictions may have reduced intervention success.
This research was supported by a grant (CA210259; Dr. David Buller, PI) from the National Cancer Institute at the National Institutes of Health. Coauthors on this poster presentation included Ms. Julia Berteletti and Ms. Mary Buller from Klein Buendel; Dr. Kimberly Henry from Colorado State University; Dr. Richard Meenan from Kaiser Permanente, and Dr. Gary Cutter from the University of Alabama.
References
- Buller, D. B., Walkosz, B. J., Buller, M. K., Wallis, A., Andersen, P. A., Scott, M. D., Eye, R., Liu, X., & Cutter, G. R. (2018). Results of a randomized trial on an intervention promoting adoption of occupational sun protection policies. American Journal of Health Promotion, 32, 1042-1053.
- Walkosz, B. J., Buller, D. B., Buller, M. K., Wallis, A., Meenan, R., Cutter, G., Andersen, P. A., & Scott, M. D. (2018). Sun safe workplaces: Effect of an occupational skin cancer prevention program on employee sun safety practices. Journal of Occupational and Environmental Medicine, 60, 900-997.
Presentation 1
Title: Adaptation of an Evidence-based Occupational Sun Safety Program for Underserved Outdoor Workers in Southwest Georgia
Presenter: Dr. Alex Morshed, Emory University

African American and Hispanic workers face unique skin cancer risks from UV exposure and are underrepresented in occupational sun safety research. This presentation reported on adaptation of an existing evidence-based sun safety program—Go Sun Smart at Work—to predominantly African American and Hispanic outdoor workers in local government employers in Southwest Georgia. The adaptation is renamed Go Sun Smart Georgia.
The systematic adaptation process was informed by Dr. Cam Escoffery’s Key Adaptation Steps (1), Implementation Research Logic Model (IRLM) (2), and the Framework for Reporting Adaptations and Modifications (3). The original intervention promotes workplace policy and education to improve sun protection and was effective in a randomized trial in Colorado (4,5). The team mapped the program and delivery using IRLM and developed an adaptation tracking tool based on Rabin et al. (6) to catalogue and make decisions about potential adaptations. The team integrated multiple sources of information to identify compatible and feasible adaptations: consultation with program experts and community partners, qualitative data collection with outdoor workers and managers at two local government employers (Jul-Sep 2023), and synthesis of literature.
The intervention includes training of peer coaches; written audit of employer sun safety policies, practices; employee training; and resource website (for example: training, sample policies, print materials, videos). In a pilot study with two local government employers, 11 employees identified by senior managers completed virtual 30-minute instruction to be peer coaches. Peer coaches delivered the sun safety training at staff meetings (21-39 employees per session). Several promising adaptations were identified, including modification of educational materials to better represent the worker population, addressing misconceptions, and use of external peer coaches at the workplace. Interviews with managers and focus groups with employees are in process.
Adaptation of existing, effective interventions to better address population characteristics and needs can increase feasibility and scalability with employers throughout Georgia, which furthers dissemination and reach of existing evidence base for improving occupational sun safety and preventing cancer.
This research was supported by a grant (U48DP006377) from the Centers for Disease Control and Prevention to the Emory University Prevention Research Center (Dr. Alex Morshed from Emory University and Dr. David Buller from Klein Buendel, MPIs). Coauthors on this oral presentation included Ms. Mary Buller, Dr. Barbara Walkosz, Ms. Irene Adjei, Mr. Brandon Herbeck, and Dr. David Buller from Klein Buendel; and Ms. Kayla Anderson, Dr. Cam Escoffery, and Radhika Agarwal from Emory University.
References
1.Escoffery et al. 2019. https://doi.org/10.1093/tbm/ibx067
2.Smith et al. 2020. https://doi.org/10.1186/s13012-020-01041-8
3.Wiltsey Stirman et al. 2019. https://doi.org/10.1186/s13012-019-0898-y
4.Buller et al. 2017. https://doi.org/10.1177/0890117117704531
5.Walkosz et al. 2018. https://doi.org/10.1097/JOM.0000000000001427
6.Rabin et al. 2018. https://doi.org/10.3389%2Ffpubh.2018.00102
Poster 2
Title: “Technology for Workplace Implementation of Solar Radiation Safety in Response to Climate Change”
Presenter: Ms. Mary Buller, Klein Buendel
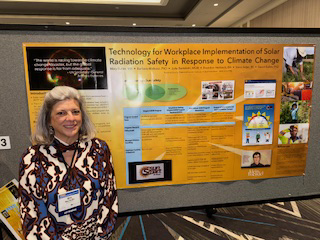
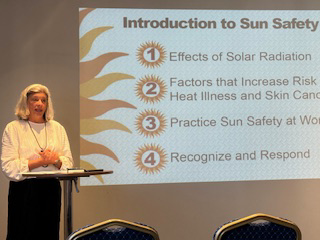
The sun’s energy is both life-saving and life-threatening. Americans who work outdoors are exposed to rising temperatures and extreme levels of ultraviolet radiation from the sun. These exposures, without preventive measures, can cause heat illness, skin cancer, and death. It is estimated that solar radiation contributed to over 350,000 deaths from excessive heat in 2019 and over 120,000 deaths from skin cancer in 2020. The U.S. government recently launched an interagency effort to combat extreme heat, including for persons who work outdoors, and the Surgeon General has identified occupational sun safety as part of a national priority for skin cancer prevention.
Workplace interviews, a review of literature and existing programs, and expert consultants helped increase dissemination potential by expanding an intervention for occupational skin cancer prevention to include heat illness prevention. Content consultants included safety training professionals, behavioral scientists, and dermatologists. The program, Go Sun Smart at Work, also includes messaging for outdoor workers of all skin types and risk profiles for both heat illness and skin cancer to be delivered online through workplace learning management systems to improve its dissemination. It will be evaluated in 2024 in a randomized controlled trial enrolling 20 worksites, their managers, and outdoor employees.
A virtual learning environment (VLE) has been programmed to disseminate and guide the implementation of comprehensive sun exposure reduction to workplaces. The VLE is a web-based program with a content database, a media platform for trackable employee training (compliant with eLearning standards), and an innovative, automated decision support tool. The tool is a chat bot-like program that customizes advice on adopting workplace policy and implementing prevention procedures to management’s readiness to innovate on sun safety based on Diffusion of Innovations Theory.
Solar radiation prevention is urgently needed to help outdoor workers adapt to a warming world. Employers have been adopting virtual training rapidly to improve accessibility, resource and learning efficiency, engagement and information retention, and fidelity and trackability. Improvements in dissemination, training, and practice, as facilitated by this VLE, can save employers time and money, improve employee health behaviors, and reduce solar-related adverse events at work.
This research was supported by a grant (CA257778; Ms. Mary Buller, PI) from the National Cancer Institute. Coauthors on this poster presentation included Dr. Barbara Walkosz, Ms. Julia Berteletti, Mr. Brandon Herbeck, Ms. Irene Adjei, and Dr. David Buller from Klein Buendel.