KB Research Presented at SBM – Part 1
Dr. David Buller from Klein Buendel presented three posters at the 46th Annual Sessions and Meeting of the Society of Behavioral Medicine in San Francisco, California, March 26-29, 2025. Dr. Kayla Nuss and Ms. Julia Berteletti from Klein Buendel were co-authors on a fourth poster.
*Klein Buendel authors are bolded.
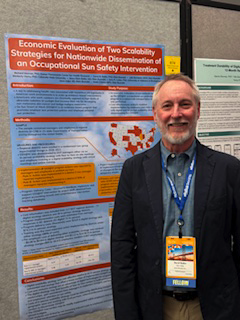
Poster 1
Title: Economic Evaluation of Two Scalability Strategies for Nationwide Dissemination of an Occupational Sun Safety Intervention
Presenter: David Buller
Authors: Richard Meenan, David Buller, Julia Berteletti, Kimberly Henry, Mary Buller, Gary Cutter, Irene Adjei, and Noah Chirico
Americans spend many hours in work environments that contribute to health risks through hazardous job exposures. An economic evaluation of two methods for scaling up the Go Sun Smart at Work (GSS@W) evidence-based occupational sun protection program to prevent skin cancer in a nationwide transportation industry was conducted. GSS@W promoted employer adoption of sun protection policies and employee use of personal sun protection.
Cost-effectiveness analysis compared digital and in-person scalability strategies for disseminating the GSS@W program in a prospective two-group randomized trial. Regional districts (n=138) in 21 state Departments of Transportation (DOT) throughout the United States were recruited. District managers were assessed before and after scale-up and employees were posttest only. GSS@W was disseminated to managers at DOT districts either via an in-person scalability strategy with face-to-face on-site meetings and employee training or a digital scalability strategy with virtual meetings and online training. Cost of delivering GSS@W was obtained from project accounting records and manager reports on number and associated costs of implemented sun protection actions. Primary cost analysis was incremental cost-effectiveness ratio (ICER) between digital and in-person strategies, using program delivery cost as numerator and number of implemented sun protection actions as denominator. Secondary analysis summarized cost of implemented sun protection actions as reported by participating districts.
Mean implemented actions per district were 6.23 in digital and 6.53 in in-person strategy groups. Program delivery costs were estimated to be $15,658 for the digital strategy and $74,275 for the in-person strategy. Across all districts, the ICER was $3,305, representing average cost savings from an action not implemented under the digital strategy but implemented under the in-person strategy. Training was the most expensive action implemented by districts under either strategy (88% of implemented action costs).
The digital scalability strategy was cost-effective relative to an in-person strategy, generating substantial cost savings and offsetting a lower mean number of implemented GSS@W program actions. The GSS@W intervention may be readily implemented within employers that manage large annual budgets. Cost analysis was limited by not assessing induced costs to employees and potential feedback effects that could produce contamination.
The research was supported by a Cancer Moonshot Initiative grant from the National Cancer Institute (CA210259; Dr. David Buller, Principal Investigator).
Poster 2
Title: Pilot Test of a Social Media Campaign on Preventing Cancer Risk Factors for Emerging Adults in Rural Communities in the American Mountain West
Presenter: David Buller
Authors: David Buller, Andrew Sussman, Echo Warner, Alishia Kinsey, Barbara Walkosz, Judith Gordon, W. Gill Woodall, Douglas Taren, Deanna Kepka, Kimberly L. Henry, Kayla Nuss, Cindy Blair, Evelinn Borrayo, David Wetter, Meghan Skiba, Julia Berteletti, Annelise Small, Dolores Guest, and John Torres
A social media campaign on preventing six cancer risk factors – being physical inactive, eating an unhealthy diet, using nicotine products, binging alcohol, being sunburned, and being unvaccinated for human papillomavirus (HPV) – was pilot-tested with emerging adults aged 18-26 living in rural counties.
Using an integrated theoretical framework, social media posts were developed to counter the cancer risk factors. Posts covered simplicity, benefits, response efficacy/cost, self-efficacy/perceived control, risk perceptions, norms, social support/relatedness, goals/values compatibility, intrinsic/extrinsic motivation, media literacy, and communication with family/friends. Twenty-six (26) emerging adults aged 18-26 living in rural counties in Arizona, Colorado, New Mexico, and Utah received a 4-week social media feed with 64 posts delivered in a private Facebook group. Emerging adults completed pretest and posttest surveys, and engagement (views, reactions, comments) was recorded.
Participants were 85% female and 35% Hispanic, with a median age of 23. At pretest, emerging adults demonstrated cancer risk factors: 53% engaged in <150 minutes of moderate-to-vigorous physical activity weekly, 85% had low daily intake of fruits and vegetables, 35% used nicotine products, 58% binged alcohol, 65% were sunburned, and 38% were unvaccinated for HPV. The campaign feed received 1,060 views, 346 reactions and 72 comments. Of the six cancer risk factors, posts on physical activity received the most views (216 views) while those on HPV and sun safety, the least (115 views each). Posts on physical activity, nicotine products, and alcohol received the most reactions (>50 reactions each) and physical activity and diet posts received the most comments (>9 comments each).
Social media is a popular source for health information among emerging adults. A multi-risk factor social media campaign has potential to engage emerging adults with theory-based cancer prevention messaging. The campaign will be evaluated in a randomized trial in 2025.
The research is supported by a grant from the National Cancer Institute (CA268037; Dr. David Buller and Dr. Andrew Sussman, Multiple Principal Investigators). Dr. Sussman is from the University of New Mexico Comprehensive Cancer Center. Other collaborating investigators are from the University of Utah, the University of Arizona, the University of Colorado, and Colorado State University.
Poster 3
Title: Association of Indoor Tanning State Laws and Other Contextual Factors with Burns from Indoor Tanning in a National Sample of US Young Adults
Presenter: David Buller
Authors: Carolyn Heckman, David Buller, Anna Mitarotondo, Daniel Gundersen, Marisa Tomaino, and Julia Berteletti
Indoor tanning by minors is a significant risk factor for the development of melanoma. In addition to FDA safety regulations, 46 states restrict minor indoor tanning access by minors to prevent acute (burns from UV exposure) and chronic (skin cancer) harms. This study’s purpose was to identify state policy and other contextual factors associated with burns from indoor tanning to inform state policy efforts.
The authors conducted an online, nationally representative survey of individuals aged 18-29 who indoor tanned in the last three years (N=1000). Respondents reported on indoor tanning as adults (age 18 or older) and as minors (under age 18). Stringency of state laws on indoor tanning use by minors was scored, with no laws regulating minor indoor tanning being a “0” and laws banning all minors under 18 from indoor tanning being a “10.” Generalized linear models were used to estimate the associations of policy stringency for minor use and enforcement, indoor tanning behavior, and other contextual factors with burns after indoor tanning as a minor or adult. All analyses used the sampling weights.
Eighty-eight percent (88%) of participants reported engaging in indoor tanning in multiple facility types in the last three years, including indoor tanning salons, gyms, beauty salons, homes, spas, and apartments. Stringency of indoor tanning laws in participants’ home states were coded as an average of 4 (weak) out of 10. Fifty-seven percent (57%) of participants reported burning one or more times from indoor tanning in the past three years, with 14% from their most recent indoor tanning session. Correlates of burns from indoor tanning when a minor were weaker age restrictions, greater enforcement, more binge drinking, tanning at locales other than an indoor tanning salon, more sessions, shorter sessions, and more sunburns. Correlates of burns from indoor tanning when an adult were being between 22-25 years old, lower perceived indoor tanning facility safety in their state, greater enforcement, more sessions, and more sunburns.
This is the first study to investigate the impact of the stringency and enforcement of age restrictions in state indoor tanning law on burns both for indoor tanning before and after age 18, in a representative national sample. Burns were very common in the context of weak laws in many states, yet harmful burns after indoor tanning during childhood appeared to be lower in states with stronger age restrictions. Enforcing weak laws or inadequate safety regulations/compliance appears to have little impact on indoor tanning or burns in minors or adults. Thus, increasing stringency of state indoor tanning laws for all facility types may ultimately decrease acute harm and subsequent skin cancer rates.
This research was supported by a grant to Rutgers University from the National Cancer Institute (CA244370; Dr. Carolyn Heckman and Dr. David Buller, Multiple Principal Investigators).
Poster 4
Title: Social Comparison as a Behavior Change Technique in Digital Interventions: Users’ Perceptions of Leaderboards to Promote Physical Activity Motivation and Behavior
Presenters: Raj Harsora and Danielle Arigo from Rowan University
Authors: Raj Harsora, Emmanuel Lapitan, Giada Benasi, Amanda Folk, Laura König, Kayla Nuss, Julia Berteletti, Kyle R. Haggerty, and Danielle Arigo
Physical activity leaderboards are a common feature in digital health tools; they display users ranked physical activity behavior from highest to lowest, leveraging social comparison to boost motivation. However, some users find them motivating while others find them aversive. It is not clear how users interpret information from a leaderboard, or for whom or under what circumstances leaderboards might be effective.
To examine these nuances, we surveyed 1,676 adults in the United States and Europe (52% women). Of those who use physical activity apps, 8% indicated that their app has a leaderboard; 70% of these users did not participate in the leaderboard and expressed dislike of this feature for its emphasis on competition, unnecessary pressure, and potential “failure.” The remaining 30% reported using the leaderboard for 2 to 24 months because it kept them motivated by showing their success, particularly as they compared to others at the “same skill level.” After viewing a leaderboard with their own rank depicted, 63% of all respondents (1,504 adults) perceived themselves as doing well with physical activity. In a separate response, however, 51% perceived themselves as doing poorly. These perceptions differed by rank but also showed meaningful heterogeneity for the same rank. Across ranks, 74% of respondents endorsed motivation to engage in physical activity though 26% did not. Physical activity motivation did not differ by rank and was not associated with perceiving oneself as doing poorly but was positively associated with perceiving oneself as doing well; the latter was strongest for those ranked 3rd of 6.
Finally, physical activity motivation in response to the leaderboard did not differ by gender but was higher among those with stronger (vs. weaker) general tendencies to respond positively and negatively to comparison opportunities; the latter did not differ by rank. Findings show that responses to physical activity leaderboards vary widely and aren’t based solely on rank or individual difference characteristics. Further, some people who believe they dislike leaderboards still find them motivating, and it is unclear how leaderboards affect physical activity behavior in daily life. Additional investigation is warranted to identify for whom and under what circumstances leaderboards are most likely to lead to benefits for physical activity.
This research was funded by an NIH Director’s New Innovator Award to Rowan University (DP2HL173857; Danielle Arigo, Principal Investigator).